We’re changing our 5th analysis into non-compliant and sanctioned facilities to focus more on trend data than current activity. This shift in focus seeks to provide our readers with more valuable insights. Our insights are based on our observations from publicly available data.
The one key piece of data we cannot get from the Commission’s data set is the rate at which initial findings of non-compliance vary from the final decision. Clearly preparing submissions is a time intensive and costly exercise. We are interested to receive feedback from any provider who has had experience in this. While the data will be anecdotal, it will provide us with some evidence that may feed into the quality improvement program of future audits. If you are happy to share your data with us, please email angie.oe@prideliving.com.au
Any information will be handled in accordance with our privacy policy.

![]()
Non-Compliance by Standard & Requirement

*Commission notice includes non-compliance notice, NTA and sanction against the quality standards
Looking across the last 12 months, we can see that non-compliances are consistently clustered around Standards 3, 7 and 8. When we drill in a little further, we can see requirements 3(3)(a), 3(3)(b), 7(3)(a), 8(3)(d), 2(3)(a) and 2(3)(e) are the ones that providers should ensure they are compliant in to reduce the risk of a non-compliance notice, NTA or sanction.
We note that the stability of the non-compliance means that the risks are known and stable. Given this, providers should be aware of the key risk areas in compliance in aged care.
![]()
Non-Compliance by Facility Characteristic
This analysis shows us where non-compliance is occurring.
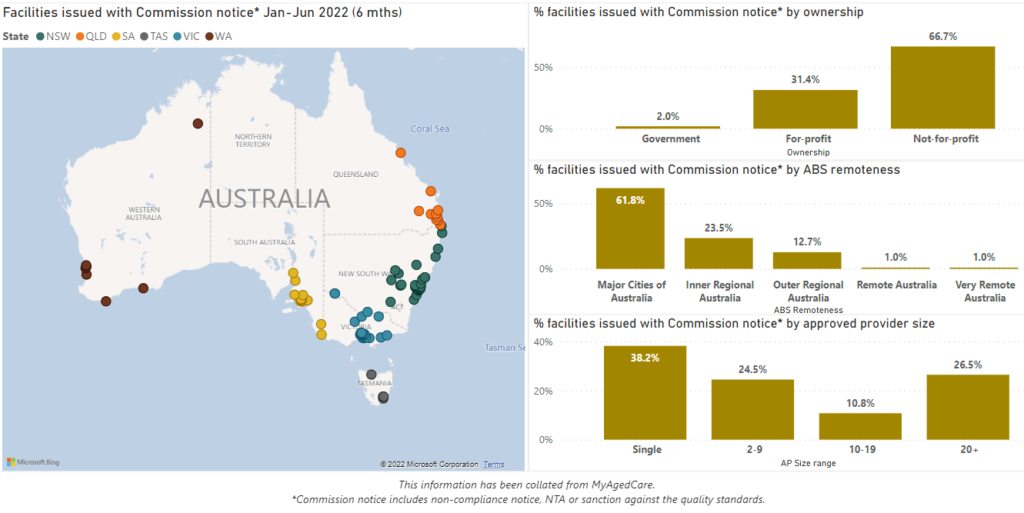

While we do not have data on the relative number of audits and assessment contacts by provider location, size and ownership, we compared the rate of non-compliance with the representation of providers.
We found that outer regional, single-site and not-for-profit providers were more likely to receive a non-compliance notice, NTA or sanction. We also found that major city, for-profit, and providers with more than 10 facilities were less likely to receive a non-compliance notice, NTA or sanction.
This suggests that having a well-resourced/funded clinical governance function is protective against these negative outcomes.
![]()
Commission Activity
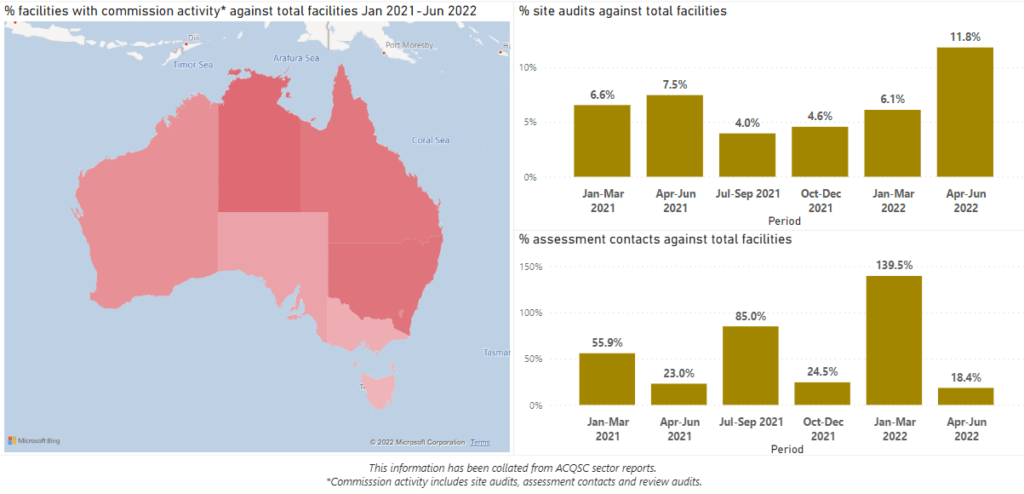
In this analysis, we are looking at where Commission activity is focused. From the map, you can see that VIC, SA and TAS are less susceptible to activity. We can also see that overall site audit activity has increased and that contact visits are sporadic, there is some correlation between contact visits and COVID outbreaks. The key takeaway from this series is that the level of audit activity is in line with the ACQSC’s strategy and a living with COVID setting.
Referring to page 27 in the ACQSC Corporate Plan 2021-22 report, the Commission reached their 2021-22 target of 2257 contact visits (actual no. of contact visits conducted: 7191) however did not meet the target of 2151 site visits (actual no. of site visits conducted: 710).
![]()
Rate of Non-Compliance

In this series, we are looking at the prevalence of activity and outcomes of that activity. Our interpretation of the results is that assessment contact activity is becoming more focused and this is resulting in a higher incidence of non-compliance, NTA and sanctions.

Key findings from our analysis:
1
There is clear and consistent evidence of which areas providers should focus their internal audit activity on if they wish to avoid a non-compliance notice, NTA and sanction
Non-compliance based on location, ownership and size shows that outer regional, not-for-profit and single-site providers are more likely to be subject to assessment contact activity.
Rather than Australia being a lucky country, Victoria is the lucky state with relatively low Commission activity and NSW is the unlucky state with proportionately higher activity.
While there is much variability in assessment contacts, presumably related to COVID outbreaks, we are seeing a consistent ramp up in audits conducted which is aligned with the Commission’s strategy.
While anecdotally we are hearing less about compliance failures, the rate of non-compliance relative to activity has more than doubled in the last 12 months – the more one looks, the more one finds

Looking forward:
1
We expect contact visits to remain at about 500 per quarter unless there are COVID outbreaks, and audit activity to continue increasing from its current base of 320
While approximately 18% of providers subject to a contact or audit will have some form of non-compliance, only 3% of providers audited (circa 15) will get either an NTA or a Sanction
3
Ensuring you are compliant in key requirements will reduce your risk of a form of non-compliance

Interactive online report
Below is an interactive online report that allows you to conduct your own analysis:

We’re here to help
At the recent ACCPA National Conference in Adelaide, Katrina Ong gave a presentation that posed the following question:
We know where the danger lies, so why aren’t we avoiding it?
Based on our interactions with providers, we suggest it is because many providers are still developing strong clinical governance practices relating to independent internal review of the key risk areas.
Some of the key learnings from our work with providers are the following:
- Focus on data quality and integrity of the QI program and SIRS
- Test your systems and ensure this is the right approach
- Culture is Key – happy staff results in happy customers
At Pride Living, we understand the demands on internal staff and the costs in resources and money to implement external internal audit programs. Based on the emerging evidence of where the systemic failures are, we’ve developed a focused Internal Review program that complements any organisations’ risk-based internal audit function. If you would like to know more about this service, contact katrina.ong@prideliving.com.au

